Humana
0→1 Human+AI Care & Benefit Ecosystem
How It Started
For many members, navigating health insurance was harder than navigating their health. Disjointed systems, call center complexity, and inefficiencies left patients frustrated and at risk. Humana saw the opportunity to reinvent the experience as a service ecosystem — one that blends human care with digital enablement to simplify access, reduce friction, and build trust.
Defining Success
Design a 0→1 healthcare navigation system that would serve all users — members, clinicians, administrators, and Nurse Navigators. This included creating an integrated service model, powered by AI-enabled triage (Nuance), with digital tools to streamline how people enter, move through, and get value from Humana’s offerings.
Making It Happen
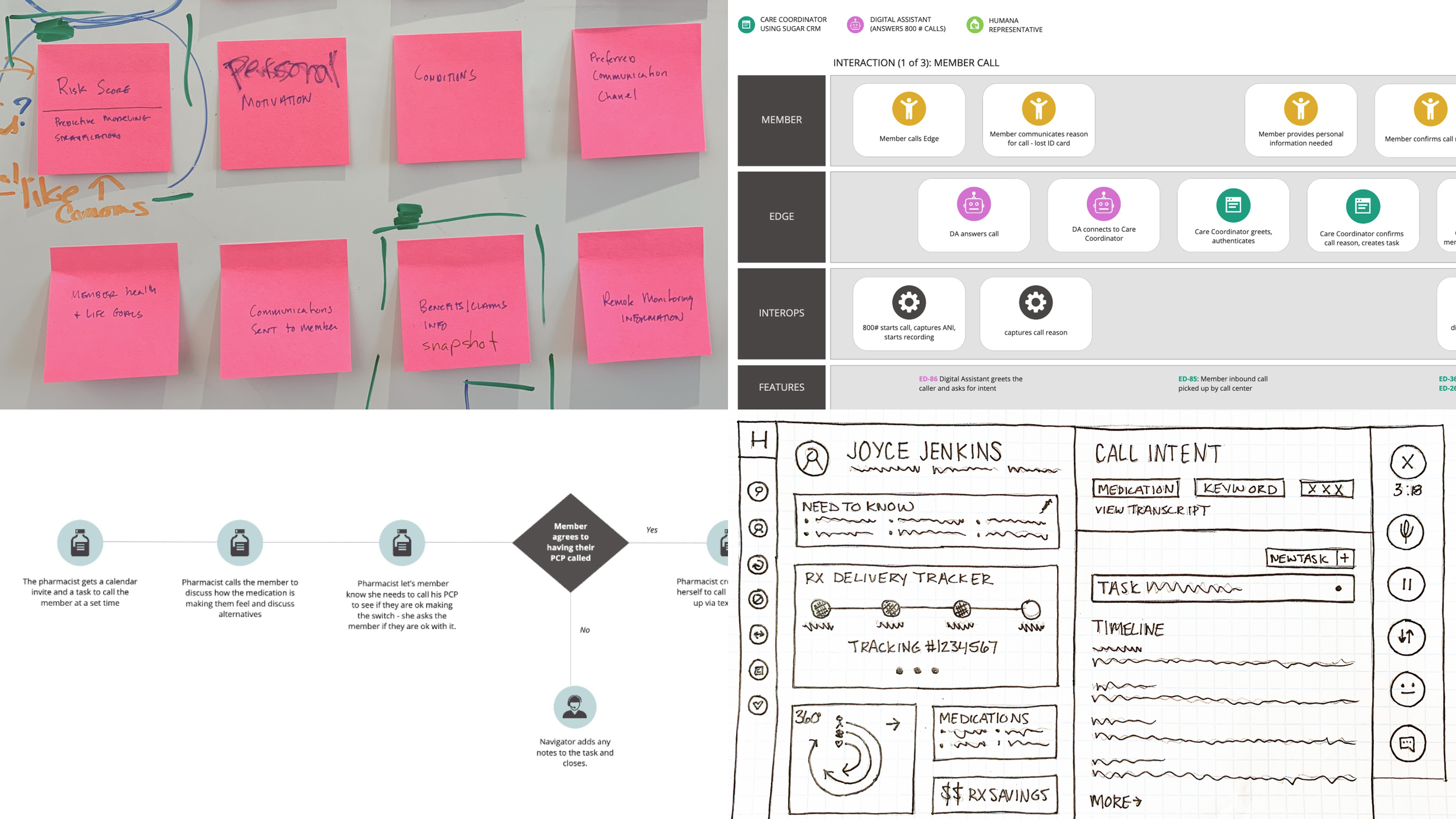
1:1 member, clinician, and admin interviews; executive and SME workshops
Macro trend analysis, SME surveys, and call center analytics
Personas, Jobs To Be Done, journey and service mapping
Co-creation workshops, storyboarding, and low- to hi-fi prototyping
Concept validation and iterative testing with multiple user groups
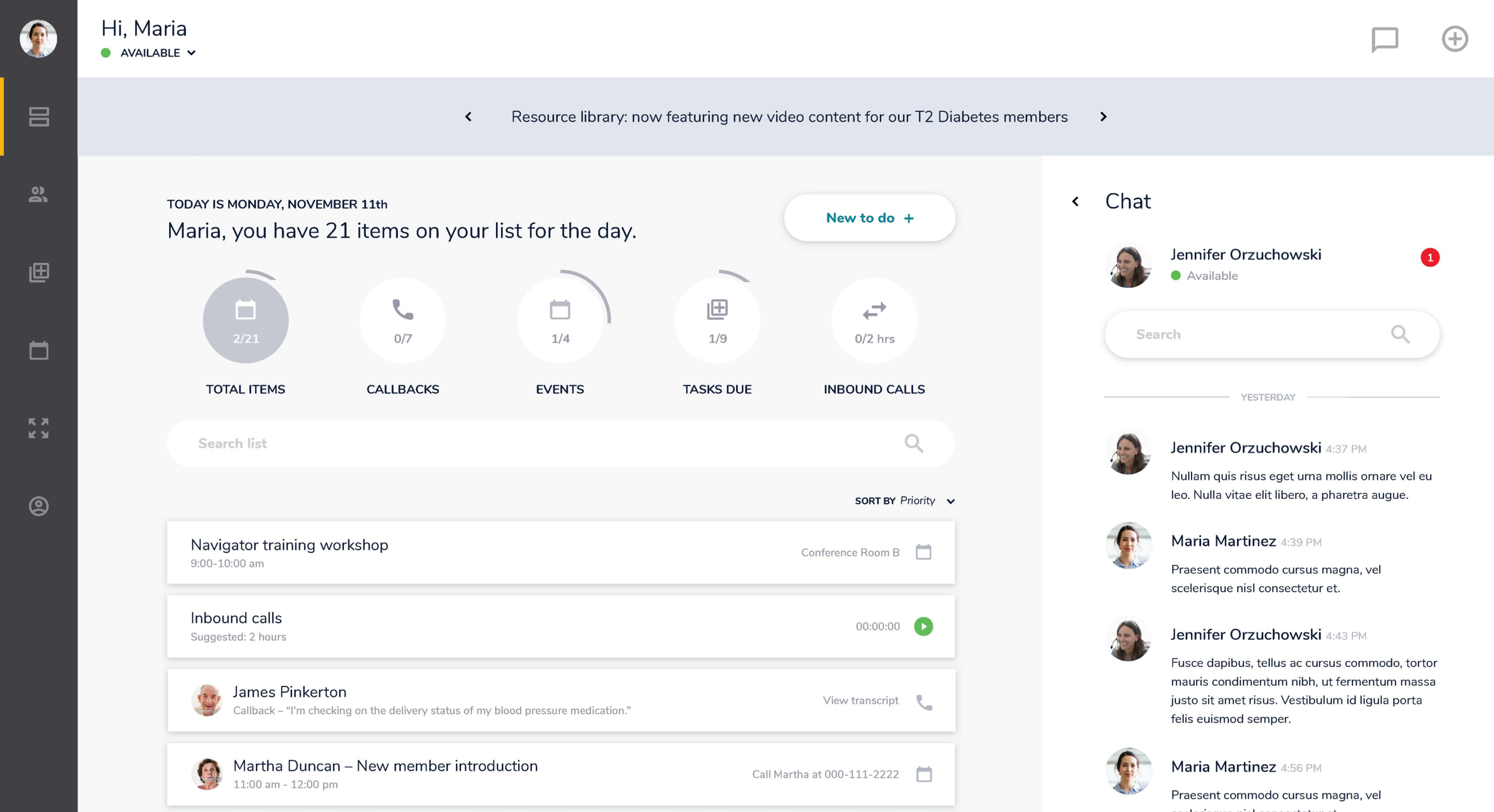
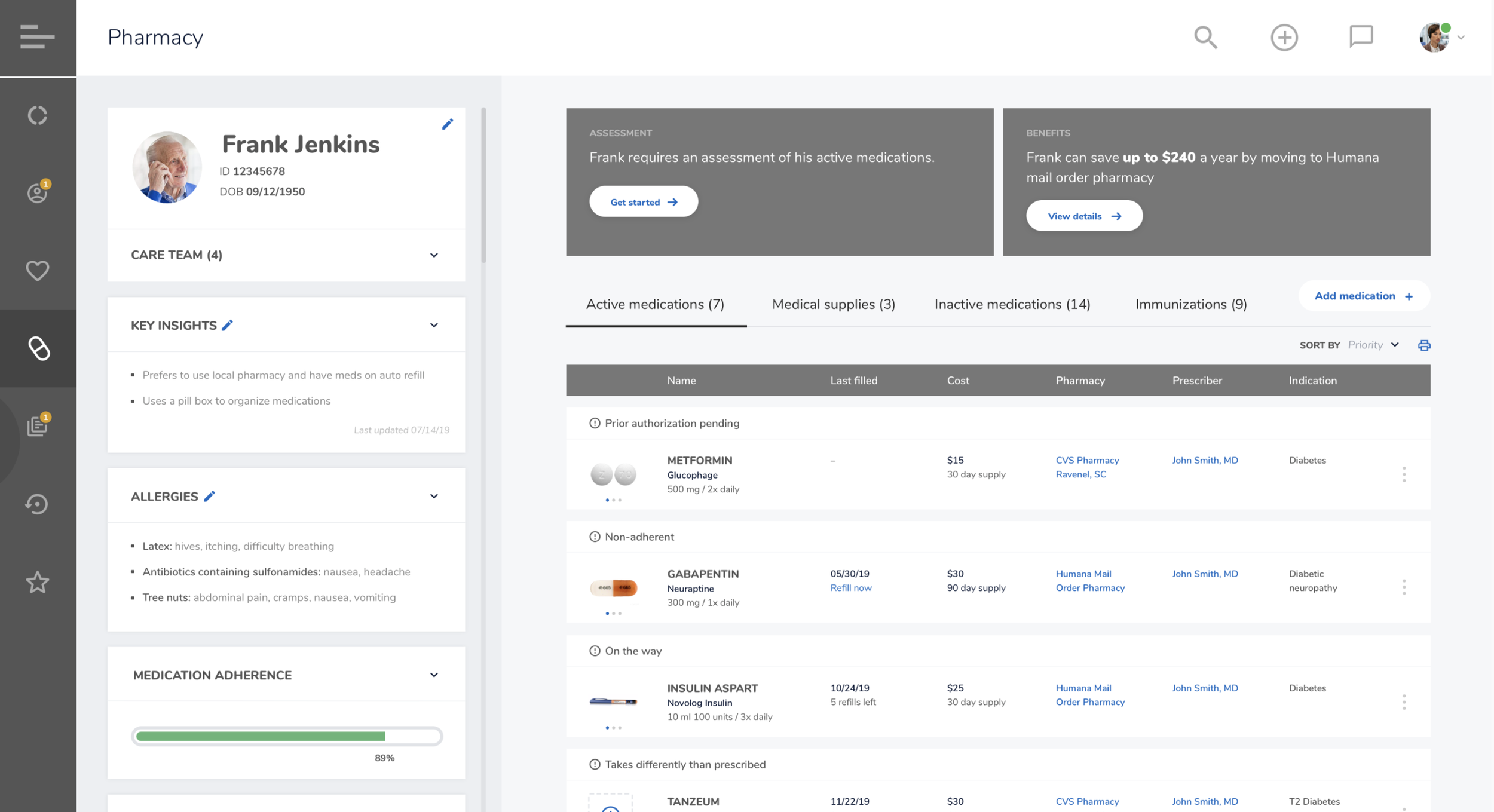
Designed mission control platform, including AI-generated “next best actions”, for Nurse Navigators to manage and escalate member care
Integrated AI triage for incoming member interactions to guide next-best-action
Production-ready UI, technical architecture planning, and agile build support
QA, usability testing, and documentation for scale
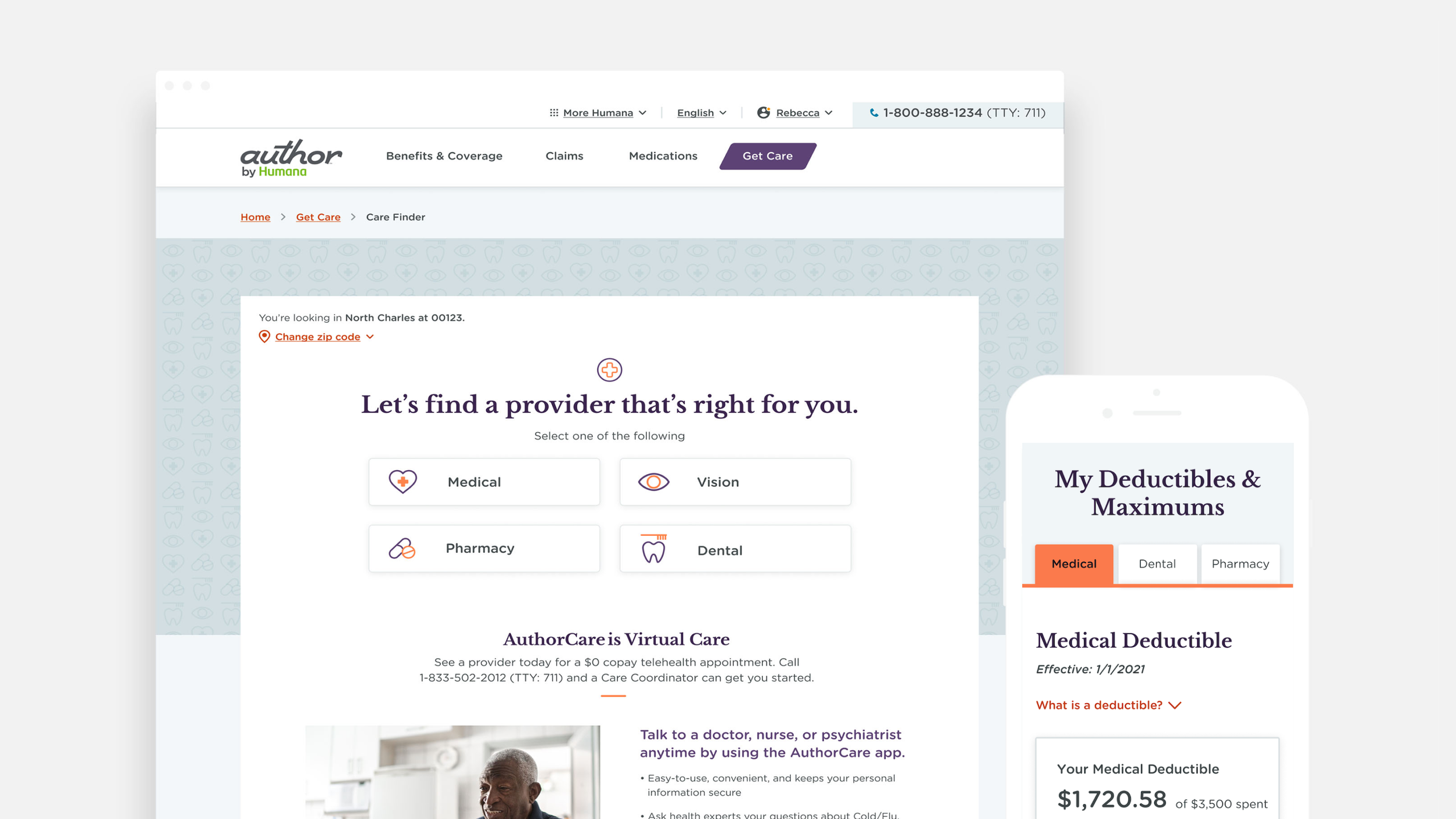
Launched Author by Humana, piloted successfully and scaled nationally across Medicare/Medicaid
Established a new model of insurer–member relationships: navigators as advocates, not gatekeepers
Positive shift in member perception — from “Humana works against me” to “Humana works for me”
Increased engagement in preventive care and benefit utilization
Reduced costs for both members and the business through streamlined navigation and escalation pathways
Outcomes That Echo